Medicare is a crucial program for millions of seniors and caregivers across the United States. However, it is also a frequent target for fraudsters, looking to exploit the system and its beneficiaries. Understanding Medicare fraud and how to protect yourself is essential for safeguarding your personal information and ensuring you continue to receive the benefits you are entitled to.

What is Medicare Fraud?
Medicare fraud encompasses a variety of fraudulent activities carried out by individuals, companies, or groups aiming to profit at the expense of the Medicare system. These activities can range from billing for services not provided to offering unnecessary services and even identity theft.
Common Types of Medicare Fraud
Medicare fraud is a serious issue that affects millions of beneficiaries and costs billions of dollars every year. Here are some of the most common types:
Billing for Services Not Provided
Providers may submit claims to Medicare for services, supplies, or equipment that were never actually given to the beneficiary. This fraudulent activity inflates the provider’s revenue while costing the Medicare system.
Unnecessary Services
Healthcare providers might offer services that are not medically necessary just to increase their billing amount. This not only wastes resources but also exposes patients to unnecessary treatments and potential harm.
Upcoding
Upcoding involves billing Medicare for a more expensive service than the one that was actually provided. For example, a routine check-up might be billed as a comprehensive examination. This practice is illegal and contributes to higher healthcare costs.
Kickbacks
Kickbacks occur when providers receive or offer something of value in exchange for referrals of Medicare patients. This unethical behavior can lead to overutilization of services and compromised patient care, as decisions are based on financial incentives rather than medical need.
Identity Theft
Identity theft in Medicare involves using a beneficiary’s information to submit fraudulent claims. This can result in the victim receiving bills for services they never received and can complicate their access to legitimate medical care.
Being aware of these common types of Medicare fraud can help beneficiaries and providers take steps to protect themselves and report suspicious activities. Combatting Medicare fraud is essential for maintaining the integrity and sustainability of the healthcare system.
The Scope of Medicare Frauds
Medicare fraud is a significant issue, with substantial financial implications. According to a report by the National Health Care Anti-Fraud Association (NHCAA), healthcare fraud costs the nation around $54 billion annually. The Government Accountability Office (GAO) also identifies Medicare as a high-risk program due to its size, complexity, and susceptibility to fraudulent activities.
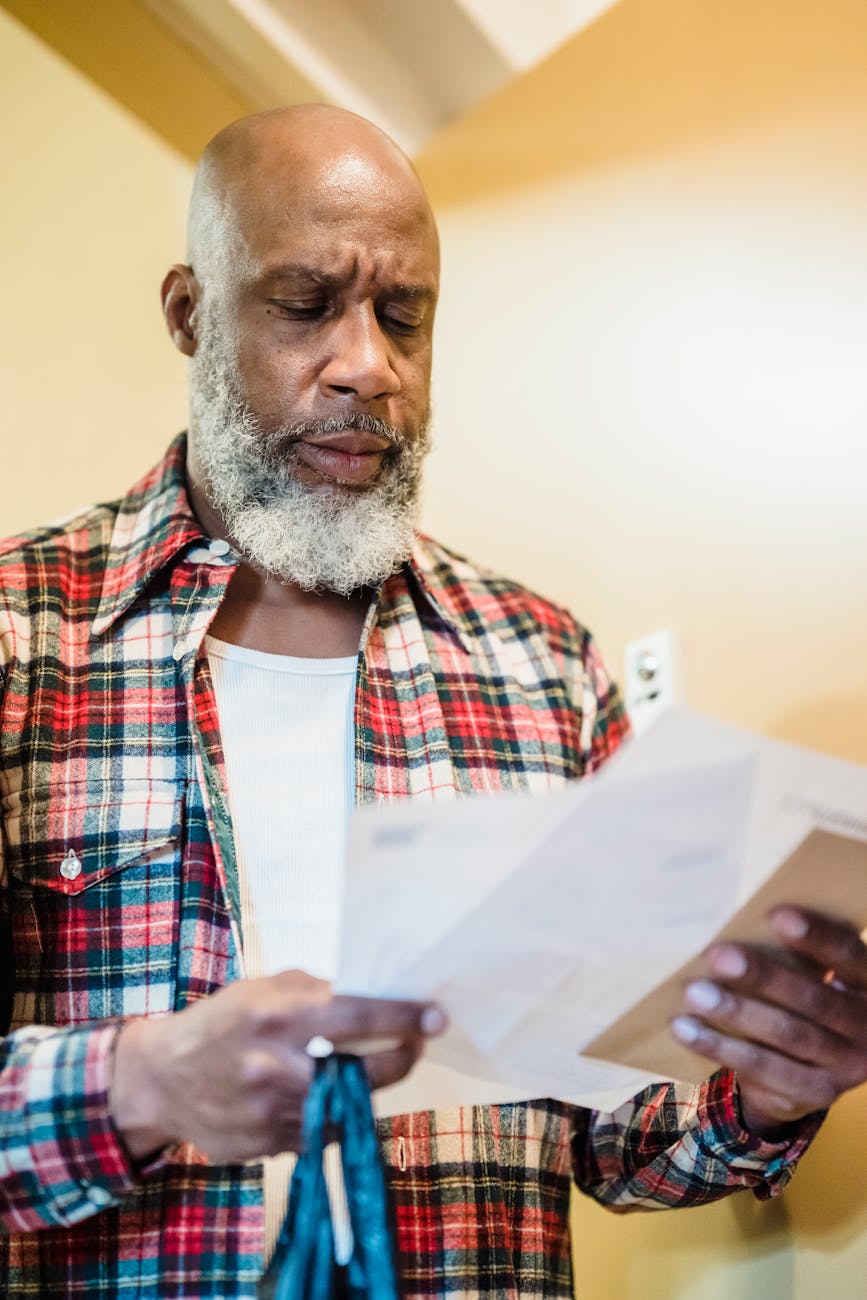
Recognizing Medicare Fraud
Medicare fraud can have serious implications, including financial loss and compromised medical care. Being vigilant and aware of the signs of Medicare fraud is the first step in protecting yourself or your loved ones. Here are some key red flags to watch out for.
Unexpected Medical Bills
Receiving unexpected medical bills is a significant warning sign. If you notice charges for services you did not receive, it could indicate fraudulent activity. Always review your medical bills and statements carefully, and report any discrepancies immediately.
Unfamiliar Provider Names
Charges from healthcare providers or suppliers you do not recognize should raise suspicion. If a provider’s name appears on your bill or Medicare summary notice and you have no recollection of receiving their services, it might be fraud. Verify the legitimacy of any unfamiliar providers with Medicare or your insurance company.
Pressure Tactics
Be wary of any situation where you feel pressured into accepting unnecessary services or medical equipment. Fraudsters often use high-pressure tactics to coerce individuals into agreeing to services they don’t need, which are then billed to Medicare.
Unsolicited Offers
Unsolicited calls or emails offering free medical services or equipment in exchange for your Medicare information are common tactics used by fraudsters. Never share your Medicare number or personal information with unverified sources. Legitimate healthcare providers will not ask for your Medicare details in exchange for free services.

How to Protect Yourself Against Medicare Fraud
Taking proactive measures to protect your Medicare information and benefits is essential. Here are some actionable steps both individuals and healthcare providers can take:
For Individuals
Monitor Your Medicare Statements:
- Regularly review your Medicare Summary Notices (MSNs) and Explanation of Benefits (EOBs) for any suspicious charges. This can help you catch errors or fraudulent claims early.
- Look for services or supplies you didn’t receive, duplicate charges, or any discrepancies in your records.
Protect Your Medicare Number:
- Treat your Medicare card and number like you would a credit card; do not share it with anyone who contacts you unsolicited. Scammers often pose as Medicare representatives, but legitimate calls or visits will never ask for your personal information unexpectedly.
- Keep your card in a safe place and only share your number with trusted healthcare providers.
Be Cautious with Personal Information:
- Avoid sharing personal or Medicare information over the phone or email unless you are sure of the recipient’s identity. Scammers may use high-pressure tactics to convince you to share sensitive information.
- Always verify the identity of the person contacting you by calling the number listed on the official Medicare website or documentation.
Report Suspected Fraud:
- If you notice any suspicious activity, report it immediately to Medicare at 1-800-MEDICARE or the Office of Inspector General (OIG) at 1-800-HHS-TIPS. Quick reporting can help stop fraudsters in their tracks and protect your benefits.
- Provide as much detail as possible when reporting, including the dates, names, and any other relevant information.
For Healthcare Providers
Implement Strong Compliance Programs:
- Establish comprehensive compliance programs that include regular training sessions for all staff members, periodic audits, and a clear, anonymous reporting process for any suspicious activities. Ensure that these programs are continuously updated to reflect changes in Medicare regulations and industry best practices.
Conduct Regular Audits:
- Regularly audit your billing practices and medical records to ensure they are accurate and in full compliance with Medicare regulations. These audits should be thorough and may involve both internal and external auditors to provide an unbiased assessment.
Educate Staff and Patients:
- Provide ongoing education to both staff and patients about how to recognize and prevent Medicare fraud. This can include workshops, informational pamphlets, and online training modules. Educating patients is equally important, as they can help identify discrepancies or suspicious activities in their billing statements.
Encourage Reporting:
- Foster an environment where employees feel comfortable and safe reporting suspected fraud without fear of retaliation. Implement a whistleblower protection policy and ensure that there are multiple channels available for reporting, such as hotlines, dedicated email addresses, or suggestion boxes.

The Importance of Vigilance
Vigilance is the key to preventing Medicare fraud. By staying informed and proactive, you can help protect yourself, your loved ones, and the Medicare system as a whole. Fraudulent activities not only drain valuable resources but also put beneficiaries at risk. Here are some additional tips to maintain vigilance:
Stay Informed:
Keep up-to-date with the latest news and updates regarding Medicare fraud and scams. Regularly check trusted websites and subscribe to newsletters that provide information on emerging threats.
Engage with Trusted Sources:
Rely on information from reputable sources such as Medicare.gov, the Office of Inspector General (OIG), and the National Health Care Anti-Fraud Association (NHCAA). These organizations offer accurate and timely information about ongoing fraud schemes and preventive measures.
Participate in Community Programs:
Engage in community programs and workshops designed to educate seniors and caregivers about Medicare fraud. These events often feature experts who can offer valuable insights and answer questions. Additionally, community involvement can foster a network of informed individuals who look out for each other.
Remaining vigilant not only helps in identifying and reporting fraud but also empowers you to make informed decisions about your healthcare. By taking these steps, you contribute to a stronger, more secure Medicare system.
It’s really problematic
Medicare fraud is a pervasive issue that requires constant vigilance and proactive measures. By understanding the different types of Medicare frauds, recognizing the signs, and taking steps to protect yourself, you can help safeguard your personal information and ensure you continue to receive the benefits you deserve.
Remember, regular monitoring of your Medicare statements and reporting any suspicious activity to the appropriate authorities are crucial steps in combating Medicare fraud.